Effectively navigating an acute (new) concussion
Written by: Dr. Cornelius van de Wall, BSc, DC, CCMI (Complete Concussion Management)
Over the last few years we’ve seen a big increase in concussion awareness. Athletes, parents, coaches, clinicians, and researchers are all paying more attention and learning how to best manage this issue. As new research emerges, old ideas are being updated and replaced. We’re already seeing a big shift in how to manage acute or new concussions compared to 10-15 years ago. This post is about updating prior knowledge and sharing information on what to expect when dealing with a new concussion, how to best manage it according to the latest research, and how to reduce risk of ongoing concussion issues.
Three key checkpoints for more effective acute concussion management
Acute concussions are defined as concussions that occurred less than 4 weeks ago (the exact cut-off varies with the study or protocol). Successful management of acute concussions is all about risk reduction. There are three key checkpoints in an individuals recovery journey, and if each checkpoint is passed through properly and safely, we expect to see full recovery within a reasonable timeline. If one or more of the checkpoints is ignored or mismanaged, the risk of ongoing concussion symptoms or multiple concussion increases.
Check point #1: On the sidelines, immediately after contact or injury
Recognizing concussion symptoms and removing an individual from play is the first important checkpoint. Awareness here has improved, but many sports teams still lack proper protocols. Some studies estimate around 50% of concussions are being missed, and we know that concussion recovery is prolonged 5-11x when an athlete continues to play in the same game (even if they don’t suffer another concussion). Knowing the signs and symptoms of a concussion is the first place to start:
Studies show that even though concussion-specific testing is helpful to diagnose a concussion (this is what we do in the office), on the sidelines new symptom onset is still the number one most accurate predictor of a concussion having occurred. After a suspicious contact or injury, all athletes and individuals should be taken aside and monitored for signs and symptoms. The presence of ANY new concussion-related signs of symptoms should mean immediate removal from play and referral to a healthcare provider.
Check point #2: Concussion Evaluation & Treatment
Next, we want to see a concussion-trained healthcare practitioner. Who you see depends on a few factors, and understanding the role of each practitioner can help guide decision making. There are three main practitioners involved in acute concussion care: an emergency room physician, a family physician, and a concussion rehabilitation professional (usually a concussion-specialist chiropractor or physiotherapist with extensive post-graduate training in concussion management).
When to go to the ER:
Immediately after the concussion if concerned, and/or if red flags (see below) are present.
Some of the signs that immediate emergency medical evaluation is needed after a concussion, head or neck trauma.
When to see your family physician:
It is nearly always recommended to touch base with your family physician after a concussion. They can help to rule out more serious issues (if that wasn’t already done at the ER), confirm a concussion diagnosis, and examine you in order to track your recovery progress over time.
When to see a concussion rehabilitation professional:
After a medical evaluation, concussion rehab is your next step. Concussion rehabilitation professionals are not usually needed to diagnose a concussion (unless you can’t get in for a medical eval). Our role is in treatment & rehabilitation of a concussion, as well as return to play testing.
In an ideal scenario, everyone would see a concussion rehab professional to help guide them through a concussion recovery within 1 week of injury. Research shows that this significantly reduces the risk ongoing concussion symptoms and multiple concussions. This is done by providing concussion-specific testing and rehab that we are trained in (we are able to go into much more detail than a general graded activity protocol), and by using objective testing to allow for safer return to play clearance (see check point 3 for this).
At minimum, it is strongly recommended to see a concussion rehabilitation professional if your concussion symptoms are persisting beyond 2-3 weeks following a new concussion, or for return to play testing for high risk sport or work.
Why see a concussion rehabilitation professional:
Reduce risk of chronic symptoms: Concussion rehabilitation professionals are able to identify early concussion-related dysfunctions that increase risk of ongoing concussion symptoms.
Quicker return to play: One study showed that those undergoing treatment were up to 4 times more likely to be medically cleared for return to play than those without treatment.
Safer return to play decisions: see check point #3 below.
Check point #3: Concussions-specific return to play testing
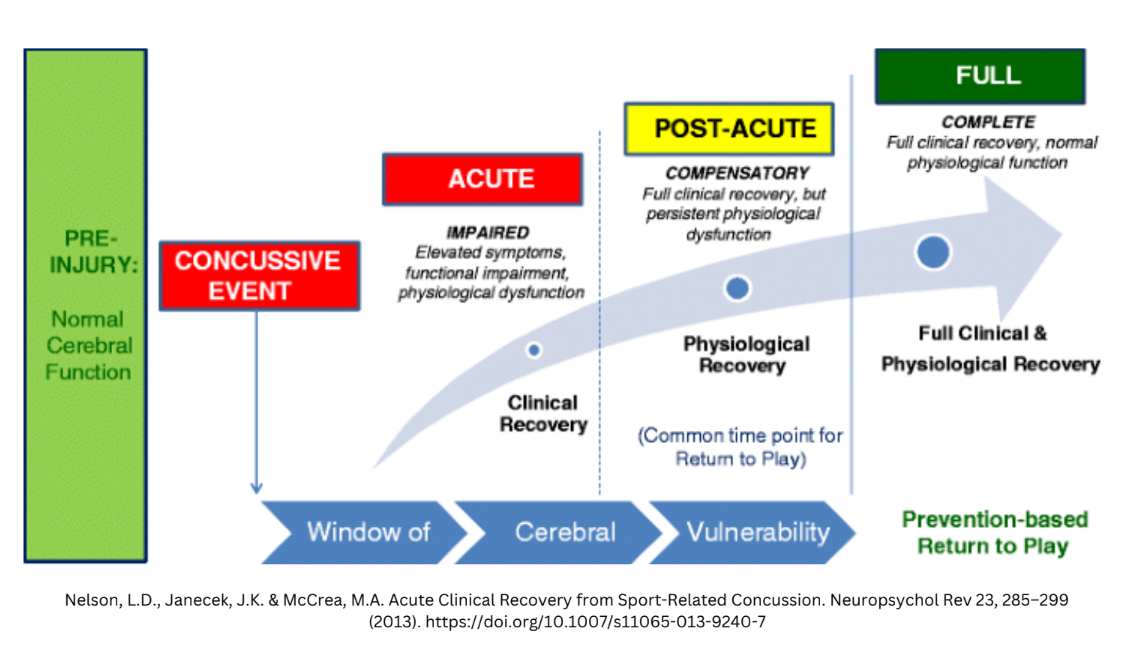
A major shift in concussion recovery is understanding that full symptom recovery and full concussion recovery are not the same thing. Previously it was thought that 90% of concussions would recover in about 2 weeks. While some athletes do report symptom resolution in 10-14 days, much more than 10% of people continue to experience symptoms beyond this timeline. Newer, more high quality studies estimate 60-70% recovery by 4 weeks as a more accurate number (with some concussion clinics publishing results as low as 50%). Studies show that regardless of what timeline symptoms resolve (known as clinical recovery), they do so before full recovery (known as physiologic recovery) has been reached. We know this because individuals who feel symptom free at rest but have not fully recovered still show concussion-related dysfunction on brain scans, physiologic marker testing, and concussion-specific testing. Physiologic recovery usually takes an additional 2 weeks after symptoms have resolved, but times can vary.
Concussion Healing Phases
This is very important because returning to play after symptom resolution but before full healing places individuals at significant risk of suffering a second and worse concussion, as well as prolonged recovery of their initial concussion. The worst case scenario, known as second-impact syndrome, is when someone suffers from a second concussion while still healing from a previous one.
Second-impact syndrome: “Second impact syndrome is a condition in which an individual experiences a second head injury before completely recovering from a prior head injury. It is thought that athletes who sustain a concussion and return to their sport early are at exceptionally high risk.” - NIH May, 2023
Safe and effective return to play decisions require symptoms to be gone as well as concussion-specific testing be negative. Concussion-specific testing usually includes exertional, visual, vestibular, and neck-related tests where are are looking to see if normal function is present and if concussion symptoms are reproduced. Only after those parameters are met can an individual be safely returned. If using symptoms alone, there is a big question mark as to whether or not full healing has occurred even if the individual has waited 4 weeks or more post concussion.
“Among players that experience two separate concussions, over 90% will experience both concussions within 10 days of each other and often will exhibit a longer duration and intensity of symptoms” - (Thomas et al., 2011)
This last checkpoint continues to be a big issue in acute concussion management, partly because return to play clearance decisions are often made based on symptoms alone, and without concussion-specific testing.
Summary
As concussion research evolves we are updating our understanding of healing times as well as ideal treatments, and as practitioners we have to stay up to date on emerging findings.
Concussions can be debilitating injuries if symptoms persist or additional concussions occur. Management of new concussions is mostly about risk reduction, with the most important checkpoints listed above. If these checkpoints are kept in mind and passed through, the risk of ongoing symptoms significantly decreases for the vast majority of people.
Are you interested in acute concussion management in Chilliwack?
Click here to find out more about Optimum Sport & Dr. van de Wall’s concussion program.